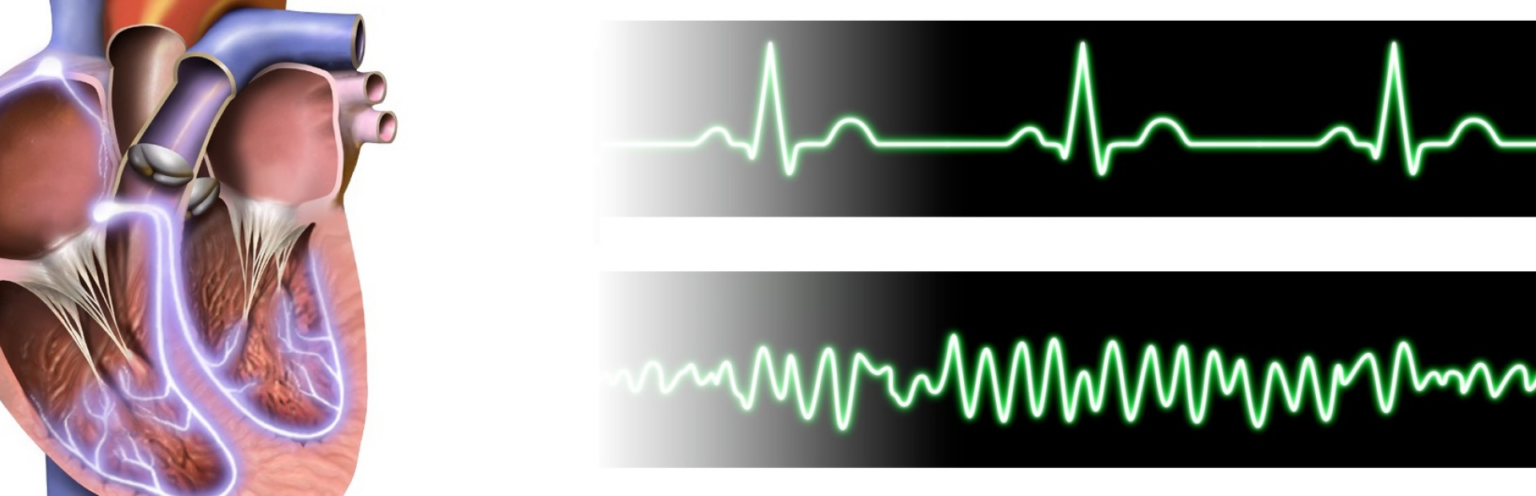
Ventricular fibrillation (VF or V-fib) is the most common initial heart rhythm in patients with out-of-hospital cardiac arrest (OHCA), and the most salvageable one.5 In VF, the etiology of arrest is often attributed to either acute ischemia or non-ischemic arrhythmia.8
Although VF appears as a chaotic and disorganized rhythm, characteristics of the ventricular fibrillation waveform such as amplitude, frequency, and organization can be systematically quantified in real-time.4 These measures have correlated with arrest physiology and are strongly related to clinical outcomes.7 Current guidelines call for prompt and repetitive defibrillation in the setting of VF during cardiac resuscitation.2 Early defibrillation is key, but its success largely depends on several other factors, including witnessing of the arrest, early bystander cardiopulmonary resuscitation (CPR) and most importantly, the time from arrest to the first shock.3
Causes
Irrespective of the cause of cardiac arrest, the most important interventions are early recognition and calling for help—including appropriate management of the deteriorating patient—early defibrillation, high-quality cardiopulmonary resuscitation (CPR) with minimal interruption of chest compressions, and treatment of reversible causes.6
The easiest way to remember the most common causes of VF are to review the reversible “Hs and Ts” in cardiac arrest. The Hs include hypoxia, hypovolemia, hypothermia, hyper/hypokalemia, and hydrogen ions (acidosis). The Ts are tension pneumothorax, cardiac tamponade, toxins, and thrombosis (pulmonary or coronary).
Ventricular fibrillation falls under the ACLS Adult Cardiac Arrest Algorithm and is the most important algorithm to know for adult resuscitation. Ventricular fibrillation treatment starts with early and effective CPR with the application of oxygen and monitor/defibrillator placement. Keeping the brain, heart, and other vital organs perfused is very important in an arrest.

Once the rhythm is identified as ventricular fibrillation, a shock should be delivered immediately. There are 2 types of defibrillators in use: biphasic and monophasic. If a monophasic defibrillator is in use, 360 joules should be delivered to the patient. If the defibrillator is biphasic, the manufacturer recommended joules should be selected (usually 120 to 200 joules). If the amount is unknown, use the maximum available and subsequent doses should be equivalent, and possibly higher.1
After the shock is delivered, begin CPR again for 2 minutes. At the beginning of the arrest, providers should be thinking about the reversible causes of cardiac arrest so treatment can be implemented according to the algorithm.
After 2 minutes of CPR, the rhythm should be reassessed during V-fib treatment. Depending on the rhythm, providers will continue the Adult Cardiac Arrest Algorithm or begin using the appropriate one. Continued VF calls for another shock, followed by good CPR once again for 2 minutes.
If the patient remains in ventricular fibrillation, pharmacological treatment should begin. Epinephrine is the first drug given and may be repeated every 3 to 5 minutes. If epinephrine is not effective, the next medication in the algorithm is amiodarone 300 mg.
Defibrillation and medication are given in an alternating fashion between cycles of 2 minutes of high-quality CPR. Continue until the patient achieves return of spontaneous circulation (ROSC) or the cardiac arrest team determines it is time to stop the resuscitation efforts.
References
- American Heart Association. Advanced cardiac life support: provider manual. United States of America: American Heart Association. 2016.
- American Heart Association. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. Part 6: advanced cardiovascular life support: section 3: adjuncts for oxygenation, ventilation and airway control. American Heart Association in collaboration with the International Liaison Committee on Resuscitation. 2000;102(Suppl. 8):I95-I104.
- Cummints R. Improving survival from sudden cardiac arrest: the chain of survival concept (a statement for health professionals from the advanced cardiac life support subcommittee and the emergency cardiac care committee). American Heart Association. 1991;83:1832-47.
- Hidano D, Coult J, Blackwood J, Fahrenbruch C, Kwok H, Kudenchuk P, Rea T. Ventricular fibrillation waveform measures and the etiology of cardiac arrest. 2016;109:71-5
- Holmberg M, Holmberg S, Herlitz J. Incidence, duration and survival of ventricular fibrillation in out-of-hospital cardiac arrest patients in Sweden. 2000;44(1):7-17.
- Truhlar A, Deakin CD, Soar J, Khalifa GE, Alfonzo A, Bierens JJ, Brattebo G, Brugger H, Dunning J, Hunyadi-Anticevic S, Koster RW, Lockey DJ, Lott C, Paal P, Perkins GD, Sandroni C, Thies KC, Zideman DA, Nolan JP. European Resuscitation Council guidelines for resuscitation 2015. 2015;95:148-201.
- Wijesekera VA, Mullany DV, Tjahjadi CA, Walters DL. Routine angiography in survivors of out of hospital cardiac arrest with return of spontaneous circulation: a single site registry. BMC Cardiovascular Disorders. 2014;14:30.
- Youngquist ST, Hartsell S, McLaren D, Hartsell S. The use of prehospital variables to predict acute coronary artery disease in failed resuscitation attempts for out-of-hospital cardiac arrest. 2015;92:82-7.
Recommended Articles

Shockable Rhythms: Ventricular Tachycardia, Ventricular Fibrillation, Supraventricular Tachycardia
According to television, if there’s a heart problem, you shock it, right? WRONG! Learn how to properly manage shockable rhythms.