Hi. Welcome back. I’m Mark from ACLS Certification Institute. In today’s video segment, we’re going to cover another Megacode algorithm. However, in this one our patient starts out in a narrow-complex tachycardia, so I want to take a few minutes and just review narrow-complex tachycardias.
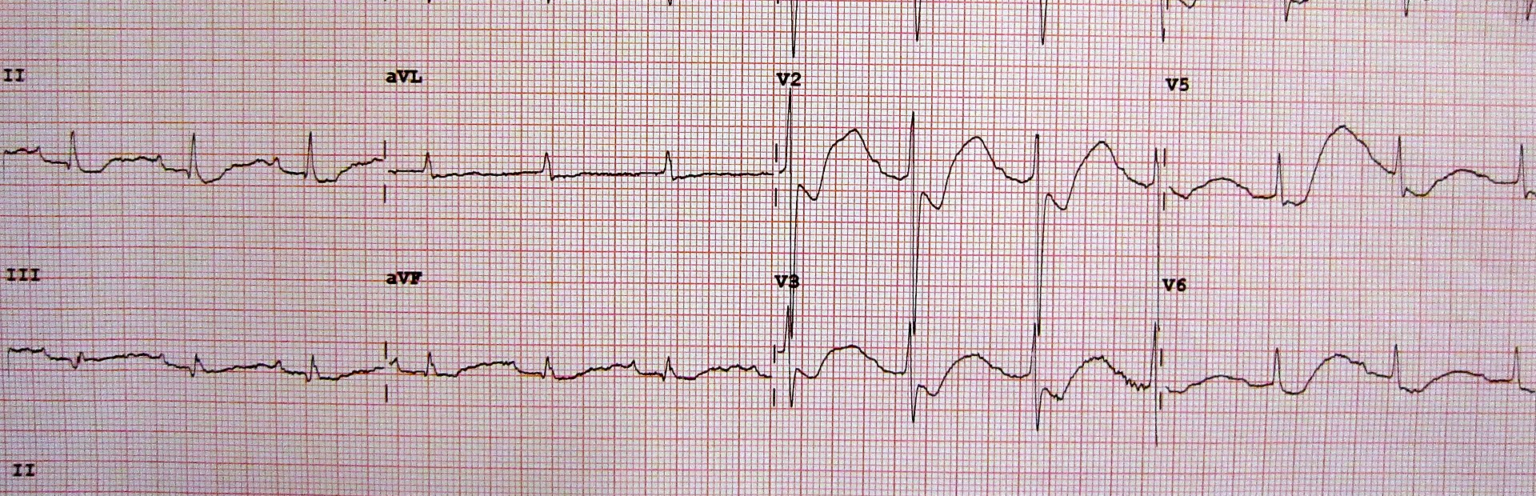
Remember, a tachycardia is any rhythm that has a ventricular rate over 100. What we’re concerned about in the adult is when the ventricular rate exceeds 150. If it’s less than 150—and I live in a world where anything can happen, but if it’s less than 150—think, is there another cause for this? Is the patient dehydrated? Are they anxious? Are they having a reaction to a drug? Is there another cause besides a primary cardiac event? If the ventricular rate’s over 150, we’re thinking, “Yeah, this could be cardiac in origin,” and we’re going to treat that appropriately. What makes a narrow-complex tachycardia a narrow-complex tachycardia? Generally, we’re looking at the width of the QRS complex. The width of the QRS complex should be less than, or at least not greater than, 0.12 seconds. If it’s greater or wider than that then it’s a wide-complex tachycardia, possibly ventricular in origin. That is a topic for another video. Let me talk about symptoms for a minute because this can be a little confusing when we’re talking about symptoms and narrow-complex tachycardia. The patient may be symptomatic. That is, to say, they have a little dizziness, may have some palpitations in their chest, but their blood pressure’s above 90 systolic. They’re not showing serious signs of shock. This is a relatively stable patient. They’re hemodynamically stable. So, we have some time. We have some wiggle room. This is the patient who’s going to receive medications. Look at the algorithm here. The first thing you notice is hypotension. This is where these other signs of shock usually arrive from. Poor skin color, altered mental status—all this comes from hemodynamic instability. This is the patient you fire up the old ‘Whack Master 3000,’ set it for sync, and give them a healthy shock.
Treating tachycardias can sometimes be confusing, so here are my tips for quick treatment of tachycardias:
Patient #1: Symptomatic, but hemodynamically stable. We’re going to treat this patient with medications, or you could try a vagal maneuver first. Have the patient bear-down, like they’re trying to squeeze out that cheese pizza. Have them purse their lips and blow out hard, like they’re trying to blow through a thin straw. Try to stimulate the vagal nerve to slow the heart rate down.
Patient #2: Symptomatic, hemodynamically unstable, systolic blood pressure less than 90. We’re going to treat this patient with immediate synchronized cardioversion. Not defibrillation. Synchronized cardioversion.
Patient #3: Narrow-complex tachycardia, no pulse. This is PEA. We’ll immediately go into our PEA algorithm.
Quick review: Symptomatic/stable, medications. Symptomatic/unstable, synchronized cardioversion. Narrow-complex tachycardia/no pulse; that’s PEA, and we’ll go into that algorithm.
Let’s go ahead and get into our Megacode scenario for today. Today we’re working in the ambulance, so let’s go ahead and beam over the ambulance, shall we.
Today we’re working pre-hospital. Our first patient of the day: 68-year-old male. You get called to the scene of a local bar. You find the gentleman sitting at the bar. You ask him what’s going on. He says about 30 minutes ago he began feeling light-headed, dizzy, came on all of a sudden. You ask him how much has he been drinking. He says he hasn’t started drinking at all. You feel his pulse, a quick radial pulse, and it feels rapid and thready. As the team leader on this call, I’m going to start assigning roles. I want the other paramedic to put him on oxygen. Let’s get him on a monitor. Let’s get some vital signs, start an IV. We get a quick blood pressure. Blood pressure’s 110/70. Respiratory rate’s about 20, is clear bilaterally. Room air SPO2 is 95%. We hook him up to the monitor and we see this: narrow-complex tachycardia with a rate of 168. He’s symptomatic, but he’s hemodynamically stable. How do we treat this? Medications. First drug of choice? Adenosine 6 mg rapid IV push. Remember when I said before that all IV medications in a cardiac arrest have to be followed with 20 cc syringe bolus of saline to help push that drug to the heart? Well, this patient hasn’t arrested yet, but we’re using adenosine. Adenosine always has to be followed with 20 cc syringe bolus to help push it to the heart. The reason is that adenosine has such a short half-life, only a few seconds. Once it’s in the body, it starts to wear off very quickly. How do you actual give this adenosine administration? Here’s how I do it. I take the adenosine, put it into the port closest to the patient. I take my 20 cc syringe of saline, put it into the next port downstream, clamp off distally, and I synchronize the administration with my partner: 3, 2, 1, I push, he pushes. We get the adenosine into the patient as quickly as we can. You have to get the adenosine to the heart as fast as you can and in the greatest concentration that you can so it has the most opportunity to work. While my partner is getting the adenosine ready and getting the IV in the patient, I ask the patient to bear-down. He lets out a little fart. It’s okay. It happens. Cleared a couple people out of the bar, but we keep going because we’re medical professionals. We get the adenosine and before we can get the adenosine out of the box and ready to go, my partner, who’s taking another blood pressure, now says his blood pressure is 80 over palp. The patient starts to look very pale, starts to roll off the bar stool. We help him down to the ground. Now that the patient has become hemodynamically unstable, we’re going to move into synchronized cardioversion immediately.
Let’s take a quick moment and review synchronized cardioversion because it is different than defibrillation. Go to whatever monitor/defibrillator you have. You’re still going to set it for defibrillation, but you have to depress the sync button. You’ll know that it’s in sync because a couple of things will happen. One, on the screen it should say “sync.” Also, you’re going to notice these little hashmarks above the R waves. That’s the monitor syncing up to the cardiac rhythm so that we don’t inadvertently shock the patient during the relative refractory period. You do that, you can cause V-fib. It’s going to synchronize the shock with the patient’s heart rate, which means in most cases, when you depress the button to discharge the defibrillator, you have to press and hold that button, unlike when you’re shocking or just defibrillating (you shock, it goes off). In synchronized cardioversion, you may have to press and hold the button, wait for the machine to sync up with the patient’s cardiac rhythm, and then it will deliver the shock.
However, when we check for a pulse, the patient is pulseless. Now we have a narrow-complex regular rhythm, but no pulse. This is PEA (pulseless electrical activity). Immediately begin chest compressions. This patient doesn’t have a pulse, which is strange because you’re seeing a regular narrow-complex rhythm on the monitor but it’s PEA. We’re going to administer medications, and we’re going to continue chest compressions. First drug of choice? Epinephrine 1:10,000 IV push. You repeat it every 3 to 5 minutes, and continue quality chest compressions. Review your H’s and T’s also. Try to figure out why this patient is in this rhythm. What is the underlying cause of that? (Hypoxia, hypovolemia, acidosis, hyper- or hypokalemia, hypothermia, coronary thrombosis, pulmonary thrombosis, cardiac tamponade, tension pneumothorax, toxins.) Continue the chest compressions. Consider an advanced airway. Does this patient need to be intubated?
Patient outcome #1: After continuing chest compressions, epinephrine administration, advanced airway, your patient never regained a pulse. He died in the back of the ambulance. It stinks. This is terrible.
Patient outcome #2: As you’re working the patient, you check for a pulse. Now you have a pulse. Your partner checks the blood pressure. You now have a blood pressure of 110/70. Fantastic.
Remember, when treating the patient with narrow-complex tachycardia, what guides your therapy is, is the patient hemodynamically stable. If there are serious signs of shock/hypotension, synchronized cardioversion. If the patient has a stable blood pressure and may be symptomatic, may be dizzy, may have chest fluttering, but is hemodynamically stable, that’s when you give the medications.
I’m Mark for ACLS Certification Institute. Thank you for watching today’s program.
Recommended Articles
Hypokalemia and Hyperkalemia
Disruption of potassium homeostasis causes hypokalemia or hyperkalemia, which can have devastating and long-lasting effects on patients. Learn how to identify and treat hypokalemia and hyperkalemia.