Transcript:
Hi. I’m Mark from ACLS Certification Institute. In today’s Megacode review, we’re covering wide-complex tachycardias.
What makes a wide-complex tachycardia different from a narrow-complex tachycardia? It’s the width of the QRS. The literature says that if the QRS width is greater than 0.12 seconds, it’s considered a wide-complex tachycardia. When in doubt, treat for V-tach. If the complex is greater than 0.12 seconds, it could be ventricular in origin. Sometimes it’s hard to discern whether it’s truly ventricular or it’s supraventricular with maybe a conduction problem that’s making the complex a little wider. The literature says when in doubt, treat for V-tach, treat as though it’s a ventricular rhythm and it’s ventricular in origin.
One of the first things you’ll do when you come to your patient is assess whether the patient is stable or unstable. This is pretty easy because whether the complex is wide or narrow, whether it’s ventricular in origin or supraventricular, if your patient is unstable, the treatment is the same: immediate synchronized cardioversion. Unstable patient, wide-complex or narrow-complex: immediate synchronized cardioversion. If the patient’s stable, you have some wiggle room. Get a 12-lead EKG. Get a closer look at this heart. The literature recommends a trial of adenosine, you can certainly give that, 6 mg IV rapid push. This will kind of help discern whether it’s atrial or ventricular in origin. If it doesn’t work, it’s probably ventricular. Again, when in doubt, treat for V-tach.
Let’s take a look at some wide complexes here. You can see they vary in morphology, but when you’re assessing it, you want to assess is this wide-complex regular or irregular. We’re looking specifically for changes in the morphology. Does this wide-complex rhythm look the same throughout the run of the rhythm? If it’s the same then it’s a monomorphic wide-complex tachycardia. If the morphology changes, if the complex changes its look then we’d call that a polymorphic wide-complex tachycardia, and the treatment’s a little different.
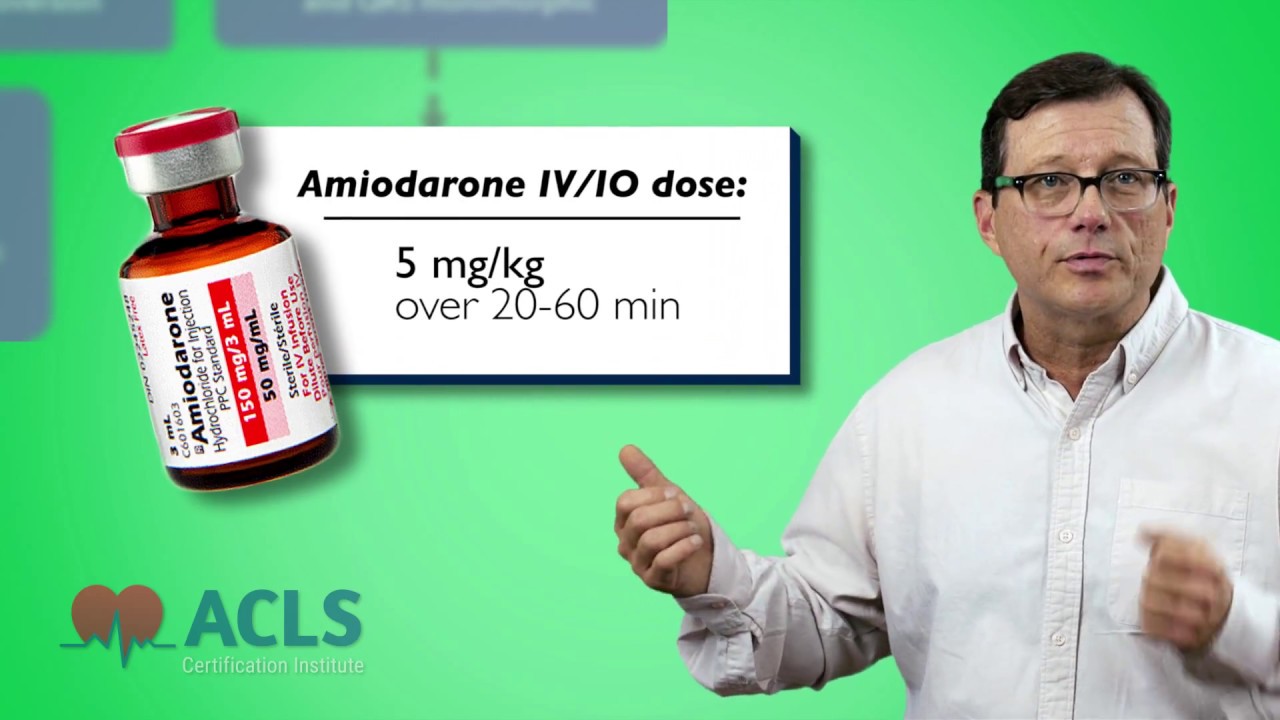
First, let’s start with monomorphic wide-complex tachycardias. In this case, we have a patient who’s in ventricular tachycardia, wide-complex ventricular tachycardia. Is the patient stable or unstable? Again, unstable means that the patient is showing serious signs of shock—low blood pressure, altered mental status, poor color, signs of shock. If that’s the case, immediate cardioversion. If the patient is stable, our first drug of choice for stable V-tach is amiodarone. Although other options exist, most commonly we’re going to be using amiodarone 150 mg administered over 10 minutes IV infusion, not a bolus. It’s administered over 10 minutes. Should the V-tach, whether it’s polymorphic or monomorphic, lapse into V-fib, which can happen, immediately go into your V-fib algorithm.
Let’s look at ventricular fibrillation. No pulse. No cardiac output. First drug of choice is epinephrine 1:10,000 1 mg IV push every 3 to 5 minutes. There’s no max on that. The first or second dose of epinephrine can be replaced with vasopressin.
Here’s your 2015 update pop-up. The American Heart Association is no longer recommending the use of vasopressin in this algorithm, only epinephrine. You can still administer epinephrine every 3 to 5 minutes, but the AHA has removed vasopressin as a pressor in this algorithm. Always follow your local protocols and your hospital policies. If they’re still using vasopressin and you’re having success then fine, but know that the AHA has removed vasopressin as a pressor in this algorithm.
Remember, when you’re running a V-fib arrest, generally drug, shock, drug, shock, drug, shock. The first drug is epinephrine or vasopressin. Defibrillate the patient. The second drug, after defibrillation, is amiodarone 300 mg rapid IV push followed with 20 cc syringe bolus of saline to push that medication to the heart. If amiodarone isn’t available, lidocaine is still a great option for V-fib. The dose is 1 to 1.5 mg/kg IV push. Repeat doses are half of that to a max of 3 mg/kg. You’ll find in the clinical setting that a lot of practitioners tend to use what works for them. I’ve run a lot of cardiac arrests using lidocaine. I’ve had good results with it, so I like lidocaine.
Let’s take a look at polymorphic wide-complex tachycardias because they’re different than monomorphic wide-complex tachycardias. Remember, with regular monomorphic tachycardias, wide or narrow, if they’re symptomatic and showing signs of shock, we cardiovert them—synchronized cardioversion. With wide-complex polymorphic tachycardias, we have to defibrillate them, usually because it won’t sync up with that. With that wide, bizarre polymorphic rhythm, the machine may not sync up to that. We don’t want to delay defibrillation or providing electrical therapy to an unstable patient. V-fib, pulseless V-tach, polymorphic wide-complex tachycardias all get defibrillated, not synchronized cardioversion; that category we defibrillate. Remember, pulseless V-tach, V-fib, wide-complex polymorphic tachycardias get defibrillated, not cardioverted.
Let’s get into our wide-complex tachycardia arrest today. We’re in the ER, and today you’re the ECRN in charge. You’re working the ER when you get a call coming in for a cardiac arrest. Let’s pop over to the ER.
ER call: “— about 2 minutes out from your facility. This is a 55-year-old male. He was witnessed to arrest at his office. Coworker started C— Stop touching that! Stop it! Sorry, we have students on board. CPR was started immediately. We’ve defibrillated him once. Patient remains in V-fib. We’re working on getting an airway and getting a line in him. Again, we’re going to be at your door in about 2 minutes.”
You’re the team leader. You know you have a V-fib arrest coming in your door in about 2 minutes. What are you going to need? You’re going to need someone to continue doing chest compressions; however, the paramedic or EMT working him is probably going to keep doing that until you’re ready and all set up. You’re going to need someone to manage the airway. You’re going to need someone to get a line into this person. Someone to administer drugs. Someone to document, to be the historian, write down what’s going on. Someone to run the code (that’s you). We see the patient coming in through the doors. When we get him in, we’re going to get him whipped over to our monitor real quick. We take a quick look at him and we see this: V-fib. Check a pulse. Again, we check for a pulse no more than 10 seconds. If patient does not have a pulse, we immediately set up for immediate defibrillation. Continue chest compressions until the defibrillator is ready to go. We shock the patient. Immediately resume chest compressions after defibrillation. Look at the monitor. The patient remains in V-fib. The nurse is telling me now we have an IV, we have an 18-guage in the right AC. The first drug of choice is epinephrine 1 mg 1:10,000 IV push. Remember to follow that with 20 cc syringe bolus of saline to push that drug to the heart. We could replace it with vasopressin. The first or second dose of epinephrine could be replaced with vasopressin 40 U, but we have the epinephrine so we give the epinephrine. Continue chest compressions for 2 minutes. The patient remains in V-fib. We defibrillate again. Immediately we start chest compressions after that defibrillation. Next drug up is amiodarone 300 mg IV push. We administer that. Continue chest compressions for 2 minutes. Look at the monitor. The patient remains in V-fib. We defibrillate again. Boom! We have a rhythm change. Any time you have a rhythm change, check a pulse. In this case, we have a pulse. It’s a regular narrow-complex pulse that we see. We check his blood pressure. Blood pressure’s 110/70. We now have an advanced airway in. We’ve intubated this patient. There’s no real guideline on when do you intubate a patient, when do you perform your advanced airway. Generally, after my second shock, I’m looking to tube the guy. I want that advanced airway. I want to make sure that I can ventilate him adequately. There’s no hard-and-fast rule on that, but generally that’s what I do. If I’ve had to shock him twice, we intubate. In this case, we have an advanced airway. The patient’s starting to buck a little bit. The doctor sedates him, and then it’s off to the cath lab to fix this guy’s heart. Nice resuscitation.
Let’s take a minute and talk about return of spontaneous circulation. We have an organized rhythm. We have a pulse. What are we going to do next? First, address the airway. Make sure the patient’s adequately oxygenated and ventilated. You want to achieve an SPO2 of at least 94%. Continuous capnography is also appropriate. Use your end-tidal CO2 to look at if this patient’s perfusing. You look at their saturation to see if they’re oxygenating. You look at your capnography to make sure they’re perfusing. Next, look at their blood pressure. Do they require blood pressure support? Do they require fluid boluses to keep the pressure up? Do we need to start a pressor infusion to keep their blood pressure up? Maintain a good blood pressure. If your hospital has the means, consider hypothermic therapy right after return of spontaneous circulation. The literature supports this, and it shows a better neurological outcome in the patient. The goal is to achieve a body temperature between 32 and 34 degrees Celsius. We can achieve this by infusing cold IV fluids, using cooling blankets underneath and on top of the patient. This should be started within minutes of a return of spontaneous circulation. Next, get a closer look at this heart. Get a 12-lead EKG. Does this patient need to be going to the cath lab? We’ve had a spontaneous return of pulse and circulation. We need to get a closer look at that heart and fix the problem. Are they having a STEMI? Are they having an ST-segment elevation myocardial infarction? Do they need to be going to the cath lab right now? Get a 12-lead. Finally, you need to get this patient up to the ICU. Start the recovery process, get this patient healed and get him home.
Thank you for watching today’s Megacode presentation on wide-complex tachycardias. My name’s Mark for ACLS Certification Institute, and I will see you in the next film.
Recommended Articles

Narrow Complex Regular Tachycardia Video
In this short video, we review narrow-complex tachycardias and ACLS algorithms. Treating tachycardias can sometimes be confusing, so here are my tips for quick treatment of tachycardias.