Hi, everyone. In this video we’re going to review the secondary assessment, which means we’ve already done our pediatric assessment triangle. The first three things we look at as soon as we see the patient: level of consciousness, color, work at breathing. We’ve gone through our primary assessment: A, B, C, D, E. Now we’re into our secondary assessment where we’re going to get more information on this patient. The secondary assessment’s broken down, really, into three parts. You have your focused history, your focused exam, and ongoing reassessment of the patient.
First, a focused history. We’re going to use the SAMPLE mnemonic. This is a mnemonic to help us remember all the items we need to get for our focused history. Starting with S: signs and symptoms. Barrier to this is obviously a 1-month-old can’t tell you what’s wrong with them, so you’re going to have to talk to the caregiver or the parent. Barrier to that is language. Do they speak English? Are you able to communicate with them so you can get an accurate history on this child? If not, you’re going to need to find an interpreter. They have great applications now for smartphones for translating languages. I can speak a language into my app, play it back to the parent or the caregiver, get an answer, and communicate with them that way. Be able to communicate with the parent. If you can’t communicate, we’re done before we even start. A stands for allergies. When we think of allergies, we tend to only think about prescribed medications. We need to think about over-the-counter medications a child might be allergic to and any foodstuffs the child might be allergic to. They get them into the hospital, we give them a sandwich, and they’re allergic to peanuts. We haven’t helped anything. Anything this child might be allergic to, we need to know about. M: medications. It’s not just what medications were prescribed by the doctor. What over-the-counter medications is the child taking? Are they taking any nutritional supplements, herbal supplements? Anything other than breakfast, lunch, or dinner that they’re putting into this child for a specific reason, we need to know about it. It might impact the care that we’re giving. It may interact with a drug that we’re giving. We need to know of all the medications and supplements this child might be taking. P: past medical history. What’s in this kid’s history we need to know about? In pediatrics, we’re always focusing on respiratory. Does the child have a history of asthma? Any breathing problems? Any cardiovascular history? Was the child term? Were they premature? These are the kind of questions we need to know in their history. Have they been sick recently? Any recent surgeries? Any pertinent past medical history we have to review. Next, L, and this is the last meal. That’s what it stands for. When was the last time this kid ate anything? Do they have any nutrition, do they have carbs, do they have energy in their body? I can tell you with the last kid I flew, a 3-month-old, throughout the course of the flight we checked this kid’s sugar three times—once in the beginning, mid-flight, and when we got there—to make sure he was not chewing up his sugars. Remember, sick kids can chew up their sugars quickly, so when was the last time they got any food in them? E stands for events. What happened? What were the events leading up to this injury or this illness in the child? This is where we have to get a clear history from the parent or the guardian as to what happened, when it happened, and how long it’s been going on, so we can put this all together and treat this kid.
Next, we need to talk about a focused examination. A focused examination is just that—we’re focusing on what the complaint is. If the child’s having trouble breathing, we’re going to focus on the chest, lung sounds, heart sounds. We’re focusing on that. We’re going to expose that area so we can focus our examination there. If the child has belly pain, we’re going to focus on that area. We’re going to listen to bowel sounds. We’re going to palpate. We’re going to assess focused on that area. After our focus exam, we can still do a brief head-to-toe assessment of this child, absolutely appropriate, but first a focused exam focusing on what the issue is with that child, especially if it’s respiratory.
Lastly, ongoing reassessment of this child. After we’re done assessing, we go back to the beginning and we start all over again. We’re constantly reassessing, looking for changes in this patient’s condition so we can pick up on it quickly and intervene quickly. Ongoing reassessment is paramount in the pediatric patient.
This has been a quick review of the secondary assessment. Thanks for watching. I’m Mark. I’ll see you in the next video.
Recommended Articles
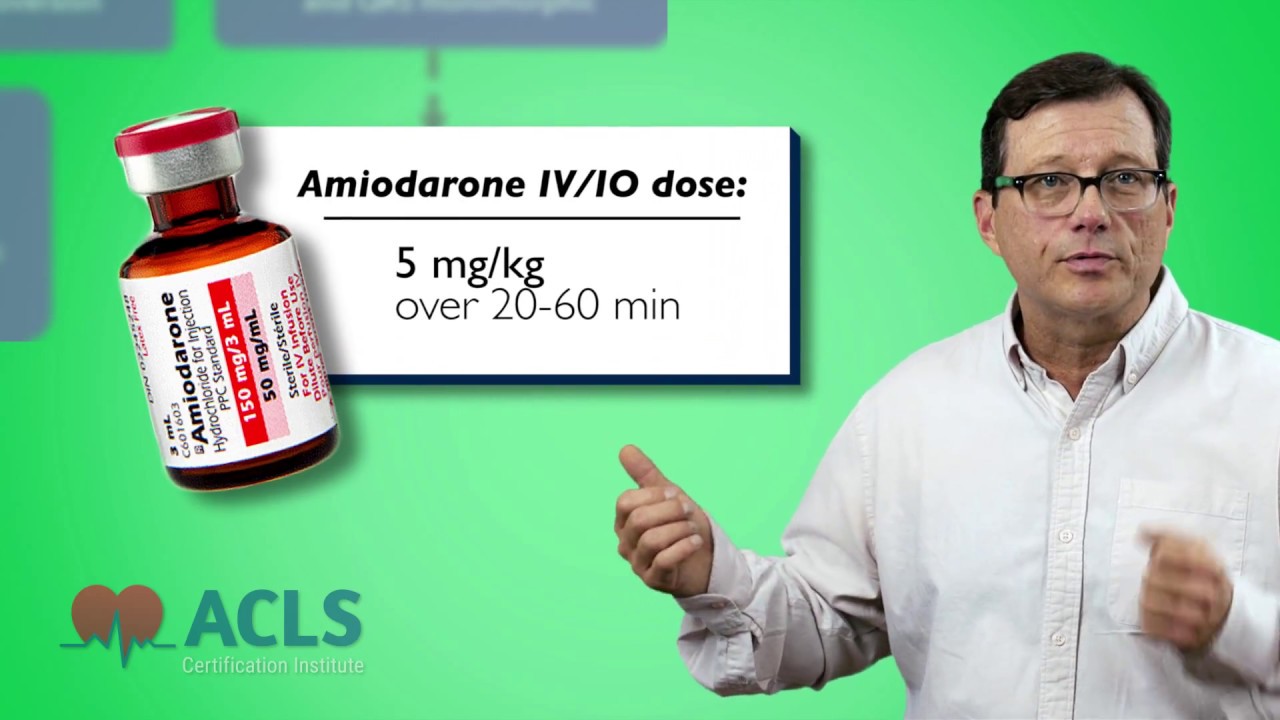
PALS Tachycardia Algorithm Video
In this video, we review the PALS pediatric tachycardia algorithm and the types of tachycardias that are seen in the algorithm.