Hi, everyone. Welcome back. In today’s video, we’re going to review the brand-new 2015 PALS pediatric tachycardia algorithm. We’re going to review the types of tachycardias that are seen in the algorithm. We’re going to talk about the causes of these tachycardias, the treatments of these tachycardias, and the drugs and drug dosages that we’re going to use to treat these tachycardias. Then we’re going to back up and look at the algorithm itself, which gives us a systematic approach to determining what kind of tachycardia we have and how we’re going to treat it. So, today, pediatric tachycardias and what you need to know. –”Ah, right in the temple. Who’s editing this? I’m standing right here. You gave me a nosebleed.”–
In this algorithm, they focus on three types of pediatric tachycardias: sinus tachycardia, supraventricular tachycardia, and wide-complex tachycardia. Sinus tachycardia you’re going to see more than any other tachycardia. You’re going to see sinus tachycardia in pediatric patients all day long. They’re very common. Less common, but you’re going to see it, is supraventricular tachycardia. Third, a wide-complex tachycardia. These aren’t very often seen in children, but you may experience them so they’re in the algorithm and we’re going to review them. Write down these three numbers: 150, 180, 220. These numbers represent the upper limits of tachycardia for the adult, for the child, and for the infant. How we use these numbers is as a guideline when we’re trying to discern between a sinus tachycardia and a supraventricular tachycardia just by looking at the rate. For instance, let’s take a look at the pediatric tachycardia of 180. If the overall rate is less than 180 in a pediatric patient, it’s usually, typically, a sinus tachycardia. If the rate is greater than 180, it’s usually, typically, a supraventricular tachycardia. Just looking across the room, if I have a 4-year-old and I can see that their ventricular rate is 220, it’s most probably an SVT. If their rate’s only 160 to 170, it’s probably a sinus tachycardia. Before we get into the specifics, you can use just the overall rate to kind of get a picture of what kind of tachycardia you’re dealing with.
First, let’s look at sinus tachycardia. What makes a sinus tachycardia a sinus tachycardia? Got one right here. Let’s take a peek at it. First, the overall rate. Notice it’s less than 180. Typically, sinus tachycardias are less than 180, a pretty good indicator. Next, the presence of a P wave. You will see a very clearly defined P wave on your ECG tracing, followed by a narrow QRS. That makes it sinus in origin. Sinus tachycardia is usually caused by compensating for something other than the heart. The heart is not typically the problem. It’s something other than the heart that’s the problem and the heart is compensating. A child will try to maintain their cardiac output, their perfusion, almost entirely by increasing their heart rate. Remember our cardiac output formula, stroke volume times heart rate? If the other problem could be a volume loss (this child has lost some volume), the body will compensate by increasing its heart rate. Causes of volume loss in a child? Vomiting, diarrhea, fever. Then you have the really icky ones: anaphylaxis or sepsis. Again, this sinus tachycardia is trying to compensate for this volume loss, and you’re going to find this during your assessment, asking Mom or the caregiver what’s been going on with this kid. If you have a 3-day history of vomiting and diarrhea, pretty good chance it’s from volume loss. Also, sinus tachycardias go along with that history. They don’t pop up all of a sudden. Usually there’s something going on with this kid for a while and they’re slowly developing this tachycardia.
Next, supraventricular tachycardia. The first thing you’re going to notice is the overall rate. Typically, SVTs in children are greater than 180. Next, no P wave. The rate’s so fast you will not see a P wave, so there’s no discernable P wave on your ECG tracing. Whereas in the sinus tachycardia the problem was something other than the heart, in an SVT the problem is the heart. Usually SVTs are caused by congenital heart defects and problems with the electrical conduction system of the heart, either an accessory pathway or a reentry pathway. The problem with this SVT, really, is the electrical conduction pathway. The conduction is coming down, then recycling again. It’s recirculating back to the top and causing this tachycardia to develop. Whereas in the sinus tachycardia you may see some variability in the R-R interval (they’re hard to pick up, but you may see some), in an SVT, typically, you don’t see any variability. The heart is on and it’s off to the races. Treatments for SVT : We know that the heart’s the problem and we have to slow this heart rate down. Remember before I was talking about cardiac output (stroke volume times heart rate). There’s a point of diminished return with an SVT. What’s happening here is the heart is beating so fast that during diastole, the time that the heart is refilling with blood, it doesn’t have enough time to adequately fill. Blood comes into the ventricle and before it can adequately fill, the heart beats again. The heart tries to fill up again—it beats again. We’re ejecting less blood out of that ventricle, and that’s really the problem with SVT. Although the culprit is the rate, it’s its negative impact on the stroke volume that’s really causing that diminished cardiac output. Treating the SVT: If the pediatric patient is stable, you can start with vagal maneuvers. Usually a bag of ice water, something over the eyes. We’re trying to stimulate a vagal response, trying to slow that heart rate down. If that doesn’t work, we can move to medications. Our first drug for SVT in a pediatric patient is adenosine, same as an adult. The dose is 0.1 mg/kg rapid IV push followed by a rapid infusion of saline bolus. Push that drug to the heart, just like an adult. First, vagal maneuvers. Next, adenosine.
Let’s take a look at a wide-complex tachycardia in a child. You won’t see this very often, but it does present so we need to talk about it. First, what makes it a wide-complex rhythm? The width of the QRS. We’re looking for a width greater than 0.09 seconds. Each small, little, tiny box on our ECG tracing is 0.04. It’s going to be a little bit greater than two small boxes, and 0.09 seconds is our threshold. Remember, an adult heart is bigger than a pediatric heart, so the electrical conduction takes longer in an adult than a child, right? Makes sense. However, we’re still using the same ECG machine with the same paper and the same timing, so our threshold, our criteria, for wide versus narrow is going to be different timing in the adult versus the child. In an adult, less or equal to 0.12 seconds. In a child, 0.09 seconds, simply because it’s a smaller heart and it takes less time for the conduction to follow a normal pathway. Again, wide-complex in a child is a QRS greater than 0.09 seconds. Causes of a wide-complex tachycardia? Usually congenital heart defects or something called channelopathies. If you remember from school when they were talking about sodium channels and calcium channels and potassium channels in the heart and the cells, there could be a defect with these channels themselves that is causing this wide-complex tachycardia. To discern this, you’re really going to need an expert consultation. This is where a pediatric cardiologist gets involved, if the culprit turns out to be channelopathies.
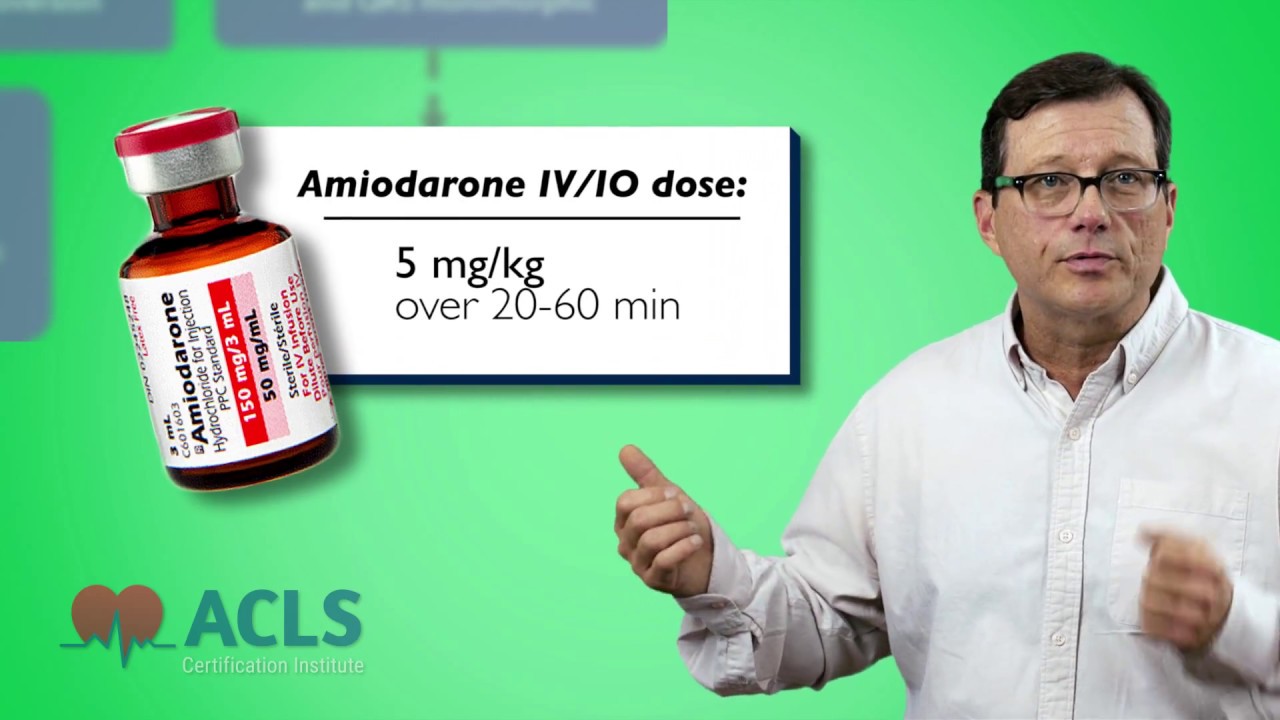
Now that we’ve looked at the different types of tachycardias, let’s back up and look at the treatment algorithm. First, the stuff we always do. Get them on oxygen, gain vascular access, and get them on a monitor. One of the first things we want to discern is if this a wide- or narrow-complex tachycardia. If the patient is stable, get a 12-lead to discern is this wide- or narrow-complex. If it’s narrow and it’s a sinus tachycardia, look for a cause and treat the cause—simple enough. Are they hypoxic? Is it volume loss? Get a history. Find the cause of the sinus tachycardia and treat it. If it’s an SVT, is the patient stable or unstable? That really guides your therapy when you’re talking about tachycardias. Stable tachycardias get treatment, medications. Unstable tachycardias—hemodynamically unstable tachycardias—get cardioverted, period. Stable: drugs or treatment. Unstable: electricity, cardioversion. Looking at the SVT part of the algorithm, if your patient is stable, you can try vagal maneuvers (the old icepack to the eyes) or you could try medications (adenosine 0.1 mg/kg), but should this SVT cause the patient to become hemodynamically unstable, immediate synchronized cardioversion. Your cardioversion dosing is half of what your defibrillation dosing would be, so you’re going to start at about 1 J/kg. Next, is this a wide-complex tachycardia? If it’s a wide-complex tachycardia and your patient is hemodynamically unstable, immediate synchronized cardioversion. Do not delay. Start at 1 J/kg and provide immediate synchronized cardioversion. If your patient has developed a wide-complex tachycardia but they’re hemodynamically stable, not showing any signs of shock (they’re stable), you’re going to use medications. You can use amiodarone 5 mg/kg infused over about 20 minutes, and you’re watching them. Make sure they remain stable. Another drug option would be procainamide 15 mg/kg over 30 to 60 minutes. Again, while you’re giving these medications, you are reassessing the patient for hemodynamic stability. Should the become unstable? Synchronized cardioversion.
This has been a review of the 2015 pediatric tachycardia algorithm. I’m Mark. Thanks for watching, and I’ll see you in the next video.