Hi, everyone. Welcome to Part 1 Introduction to Basic Life Support. In the upcoming video series, we’re going to be covering all these topics you see here, but today we’re going to focus on the key points of performing basic life support. This is important because the science suggests we do this for our patient, and, too, you may be seeing this information on a test in your immediate future. Let’s get started.
First, quality chest compressions. When performing chest compressions on the adult, the compression depth is important. The literature states at least 2 inches in the adult, not to exceed 2.4 inches. Compression rate: The new 2015 guideline specifies chest compressions should be performed between 100 and 120 compressions per minute. Remember, it’s important to allow for complete chest recoil. We see this all the time, especially in the adult. We’re leaning over the body, we’re pressing down, and we’re not allowing that chest to completely recoil. That is imperative. Again, at least 2 inches, not to exceed 2.4 inches, but we have to let that chest completely recoil before we apply the next compression. The new guidelines also deemphasize checking for a pulse. When we do check for a pulse, no more than 10 seconds, that’s it.
Next, minimize chest compression interruption. This is what they’re talking about when you hear compression fraction. Compression fraction is the time that we spend actually compressing the chest. That should be at least, minimally, 60% of the time. Within 1 minute, 60% of that 1 minute, at least, should be spent actively compressing, actively doing chest compressions.
Effective breathing for the patient, effective bag-valve-mask ventilation—what’s important to note here? Don’t over-bag the patient. Excessive breaths, excessive tidal volume can actually increase intrathoracic pressure and reduce blood return to the heart. If you’re bagging too fast, too aggressively, with too much tidal volume, more air can go into the belly. This can lead to vomiting and aspiration. We’ve gone from the frying pan into the fire, so watch your bagging. Our goal is to see chest rise, that’s it. We just want to see that chest come up and down when we apply positive pressure ventilation.
Next, the chain of survival. Honestly, if more Americans just knew this, we would save more lives. Let’s look at the adult chain of survival. First, establish unresponsiveness. Poke your victim with a stick, a sternal rub. They’re unresponsive. Next, activate EMS. Get some help coming. You’re going to need help, and you’re going to need a defibrillator. If you’re alone—one rescuer, just yourself—if you have a cell phone, pull it out, call 9-1-1, put it on speaker, and go to work. If you don’t have a cell phone, you’re going to have to leave the victim and call 9-1-1. If you know where a defibrillator is, if you know where that AED is, go grab it and bring it back to the patient. If there are two rescuers, one is going to go for help and an AED, the other one is going to stay and immediately begin chest compressions. This leads us to the next step in the chain of survival, CAB (compressions, airway, breathing). Start the resuscitation. Begin chest compressions. As soon as an AED becomes available, apply it to the patient. If they need to be shocked, deliver the shock. Next in the chain of survival is early access to advanced cardiac life support. This is 9-1-1 showing up at the scene. It’s important that we get help here quickly to that victim. That’s why we call so early in the algorithm. In the chain of survival, the second step is call for help. Last step in the chain of survival is post cardiac arrest care. This is making sure we’re taking the patient to a facility that can manage a cardiac arrest and manage this patient after the cardiac arrest.
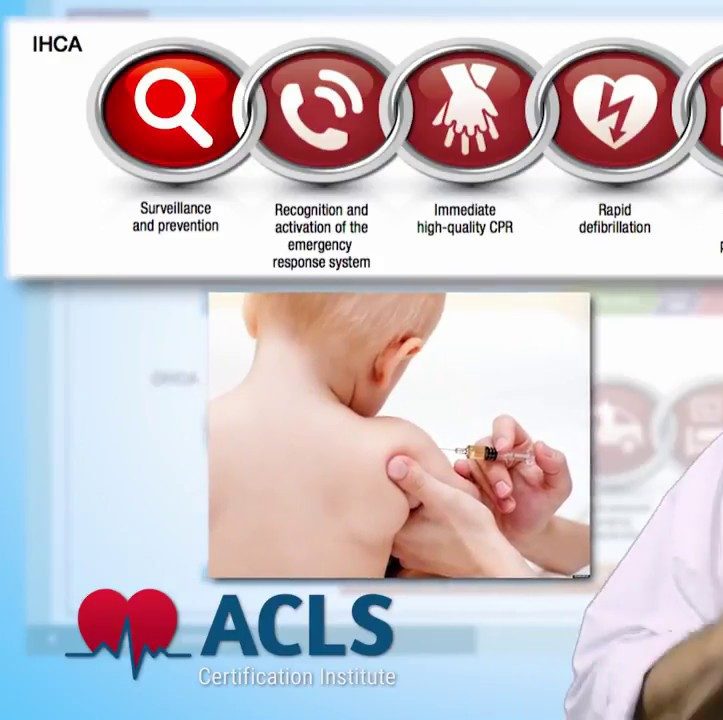
Let’s take a quick look at the pediatric chain of survival. This all starts with prevention, not letting the child arrest in the first place. Child-proofing the home, car seats, immunizations—all these things help minimize the risk of a child getting into trouble, having a cardiac arrest. Next, the emphasis is quality chest compressions, quality ventilations. Remember, when we’re compressing the chest of a child or an infant, the depth, the amount that we’re going to compress, is about 1/3 the distance anterior to posterior. Next, get help coming. Call 9-1-1. Get professional help coming quick. Next, post resuscitation care. We need to make certain that this pediatric patient goes to a facility that knows how to manage a post cardiac arrest pediatric patient.
Next, is this patient an overdose? Have they suffered from a heroin or opioid overdose? We need to assess for that quickly. Remember, these drugs are potent respiratory depressants. The patient stops breathing, then subsequently, cardiac arrest. We need to assess for an overdose quickly and apply the antidote Narcan (naloxone) if we have it.
A few things healthcare providers specifically should be aware of: They no longer recommend the routine use of cricoid pressure during positive pressure ventilation. Whenever possible, if you have to defibrillate a child, use pediatric pads with the pediatric attenuator. If you don’t have that, if you don’t have a manual defibrillator, if all you have is an adult AED to use on this pediatric patient, then use that.
This has been Part 1 Introduction to Basic Life Support. Thank you for watching. My name is Mark. I will see you in the next video.
Recommended Articles

BLS Adult Cardiac Arrest Algorithm
The BLS Healthcare Provider Adult Cardiac Arrest Algorithm shows the steps single rescuers and multiple rescuers should take in the treatment of an unresponsive adult.