Hi. I’m Mark from ACLS Certification Institute. We’re going to begin today’s segment with a new segment we call ACLS Mailbox. Sometimes we get comments back, and we want to address a few of those in our video program.
One comment from a viewer came back as, “Great video… Why did the presenter use cc after lidocaine?” I can tell you I use cc because I’m old. The new trend now is a couple years ago they wanted to replace cc with mL when describing fluid administration, and I agree with that. It’s more precise. The mL stands for milliliters, and it denotes an amount of fluid. The cc stands for cubic centimeters, and it more denotes an amount of space. Know that 1 mL of fluid will occupy 1 cc of space. In the end, they are almost interchangeable. For years and years and years, I’ve been saying cc. Now the new guide lines use mL. Am I going to change? Probably not. I’ve been saying cc for 20 years—that’s a hard habit to break. Should you be working a cardiac arrest with the head of Cardiology, and he says, “Go ahead and administer 10 cc of 10 % calcium chloride,” give it. You don’t have to correct him right there. If you want to correct him afterwards, that’s fine (invite me, I’d love to see it), but there’s no need to. Is cc and mL important for testing? Most definitely, use mL. In your documentation, use mL. But if cc slips out of somebody’s mouth, know that they mean mL. Excellent suggestion. Thank you very much.
Keep those comments coming. We appreciate them, and we look at all of them. This concludes today’s Mailbox.
*****
Hi. I’m Mark for ACLS Certification Institute. In today’s program, we’re going to talk about drug calculations—how to draw it up correctly and administer the proper dose of medication to your patient. First, let’s take a look at the drug packaging.
First, you’re going to have the name of the drug (very helpful). Second, you’re going to have the total amount of drug in that container. Then you’re going to have the total amount of fluid that’s in that container. Then you’re going to have the concentration. The concentration is how much drug per cc is in that container. You’re going to need to know all of these so that you can accurately calculate and administer the drugs. It seems about every 8 minutes in EMS, someone’s coming up with a new acronym, a new mnemonic, flip chart, field guide, something scribbled on cocktail napkin with a formula so we can remember how to do stuff. Formulas are great. I’m going to share with you today some formulas that I learned for calculating medications.
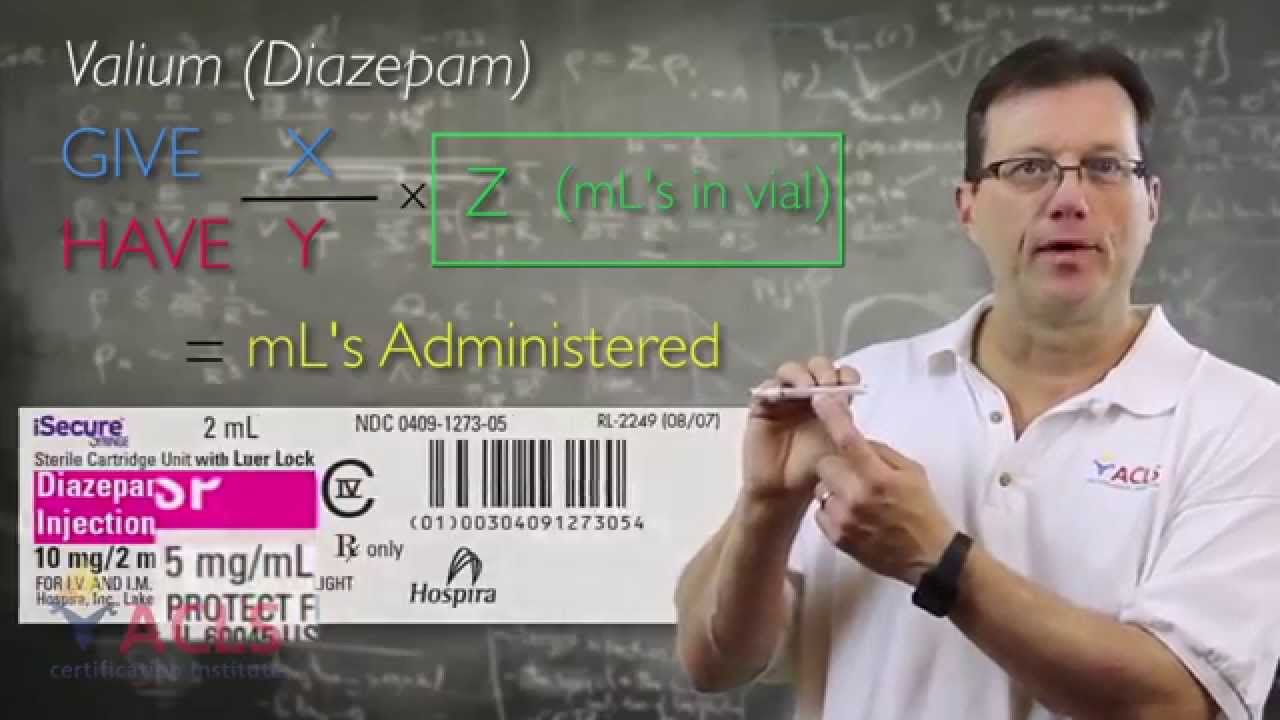
For simple injectables, for one-time shots, remember the formula ‘give’ divided by ‘have’ times ‘cc in the vial’ equals ‘cc administered.’ Let’s break that down a little bit. Give divided by have. Give: When I’m talking about give, I’m talking about how much drug do I want to administer to that patient, and that’s the dose. The dose is how much drug I’m giving to the patient; not how many cc, but how much drug am I administering to the patient. How much drug do I want to give, divide that by how much drug do I have—what’s the total amount of drug in this vial? Give divided by have times cc in the vial, and that remains constant. Even if you start drawing fluid or medication out of that vial, the number of cc in that vial remains the same because that’s the concentration. For example, if you have 4 mL in 2 cc and you pull out 1 cc, it’s still 2 cc. You don’t subtract that amount. Whatever is written on the vial, that remains constant throughout the administration of the drug or repeat administration of the drug. Remember, give divided by have times cc in the vial equals the amount of cc we draw up to administer that dose.
Let’s take a look at that and run through a practice here. Say we have a patient and we’ve worked them, we’ve resuscitated them, but now they’re going to need some sedation. I have some Valium here and I have 10 mg in 2 mL. It gives me the total amount of drug, which is 10 mg, the total amount of fluid, which is 2 mL, and it also gives me the concentration, which is 5 mg/mL. The doctor says, “Okay, give him 4 of Valium.” Okay, 4 of Valium—how much do I want to give the patient? I want to give the patient 4 mg; that’s the dose of medication. I’m going to divide that by how much drug do I have, which is 10 mg, so 4 divided by 10 equals 0.4. Then I take that 0.4 and I multiply it by the number of cc in this vial, which is 2. That gives me 0.8. That means that I’m going to draw up 0.8 mL to administer that 4 mg of valium.
Let’s do some practice for a minute. Let’s use that formula: give divided by have times cc in the vial. I’m going to give you some drug orders. You go ahead and work up the problems and see if you get the right answers.
Let’s talk about calculating for medication infusions now. I’ll use the example of dopamine. The first thing we have to calculate for or figure out is our concentration. You want it to be your dosing concentration, your working concentration. We all know the starting dose of dopamine for heart failure is about 5 mcg/kg/min. This bag’s going to come 400 mg in 250, but I’m dosing in micrograms so I need my concentration in micrograms. I can simply look it up on the package and it gives me that, 1600 mcg/mL; that’s my concentration. If this wasn’t on here, I can still figure it out. I just take my 400 mg, divide it by 250, and that gives me 1.6 mg/mL. I’m dosing in micrograms, so I have to have the same dosing parameters. I need to know my concentration of what I’m dosing in. In this case it’s micrograms, so I multiply that 1.6 by 1000 and I get my 1600 mcg/mL. That’s the first thing you have to calculate for—what is my working concentration. For dopamine, simply over that write down what you want—what do you want to administer the patient? I want to give 5 mcg/kg/min. The patient weighs 70 kg. Simply write that down: 5 times 70 times 60 (because it’s per minute), divide that by my concentration, which is 1600, and that will equal my mL/hr. All infusion pumps are set, ultimately, to administer mL/hr. That’s what we’re calculating for—how many mL/hr am I going to administer to achieve that dose of 5 mcg/kg/min. Let’s say we’re going to start at 10 mcg and the patient weighs 80 kg. Okay, 10 times 80 times 60, divided by my concentration equals mL/hr. Here’s a nifty little trick. Let’s say that the drug isn’t weight-based, it’s just per minute. Take that part out. Same formula.
Using this method, let’s calculate up some different dopamine drips. Again, I’ll give you a dosing parameter from the doctor. Pause the video if you need to while you’re working on your answer. Let’s work on a couple of problems.
Drug preparations come in all different kinds of sizes and packaging, but what I want to focus on right now is called the Carpuject. If you’re not familiar with these, let me just go through and show you how these guys work. Carpuject is a prefilled syringe, and it is designed to go into this actuator. You slide this in, and this little white part is going to fit into this groove here. How do you activate the Carpuject?
You’re going to screw in the bottom, and by turning this lever at the bottom and locking it in, it pulls this white tab into the vial. There’s a small needle inside here that punctures the little membrane and allows the drug to be administered. What has to happen is this white part has to be pushed down to actuate and get that needle inside the vial so we can administer the medication. To remove it, simply unlock it, unscrew it, and the whole thing will pop out.
I’m not a math whiz. I have a calculator watch on my wrist for a reason. We have to use technology. With some of these bigger calculations, especially with multiple drips, you want to double-check your work, which means you’re going to have to have a calculator. Make sure you have the right drug, the right patient, the right route, the right time, the right documentation. Have someone else double-check your work. Seriously. Is this Versed? Oh, it’s vecuronium? Yikes! Double-check your medications. Don’t be afraid to ask. Have someone physically look and double-check that medication before you administer it.
I hope these formulas help. I hope you had a good time. I’m Mark for ACLS Certification Institute, and I’ll see you in the next video.
Recommended Articles

Conscious Sedation for Cardioversion
No matter the location, DCCV is an uncomfortable procedure. Learn about conscious sedation for cardioversion and keeping patients comfortable.

ICU Nurses: Our Unsung Heroes and How They Succeed
Intense training and intense experiences motivate ICU nurses to continue their critical care nursing. Check out just how they succeed!

Managing Respiratory Arrest
Knowing and understanding the signs and symptoms of respiratory distress, failure, and arrest is crucial. Respiratory arrest is usually the endpoint of respiratory distress that leads to respiratory failure. Respiratory distress and failure have multiple causes, all of which, if left untreated, can deteriorate into respiratory arrest. The best treatment is knowing and understanding the signs and symptoms of respiratory distress and respiratory failure so interventions can be initiated and respiratory arrest averted altogether.